What is Outreach & Enrollment?
Outreach & Enrollment is a national initiative to spread awareness about the Patient Protection and Affordable Care Act (ACA), to increase the number of insured Americans. The ACA was passed by the Obama Administration in 2010, becoming law in 2013.
Why is having access to health insurance so important?
Insurance affords Hoosiers a financial blanket to obtain medical services. When a Hoosier does not have health insurance their ability to receive health care is limited due to financial burden.
Indiana Navigators
Navigators are individuals licensed by the State of Indiana specifically to provide unbiased and free advisory services to all Hoosiers, to assist with enrollment into Medicaid. Many times these individuals are also Certified Application Counselors (CAC's assist with MarketPlace) SHIP Counselors (Medicare enrollment) and Community Health Workers (CHW). They are often times found in Community Health Centers, Hospitals, Schools, etc.
The staff at IPHCA understands the importance of Hoosiers having access to health coverage and collaborates in all parts of the health care process. This includes providing training to navigators and other enrollment personnel and the community at large. Our Outreach & Enrollment division is committed to working with all Hoosiers to ensure that every Hoosier has access to affordable and comprehensive health coverage.
Save the date for Navigator Monday 2026!
Monday May 11, 2026
Look out for more details soon...
IPHCA Outreach & Enrollment is led by
Jenny Walden, Indiana Navigator, CAC, SHIP, CCHW
Jenny Walden has over 25 years of benefit enrollment experience, including health, dental, retirement plans, and other employer benefit programs. Prior to joining IPHCA in 2018, Jenny spent 10 years developing Outreach and Enrollment teams within Federally Qualified Health Centers. Her expertise is supporting Outreach and Enrollment teams in health centers by using her knowledge of state and federally funded programs, such as HIP 2.0, Medicaid, SNAP, TANF, Marketplace, and SSI/SSDI.
Find out more about our work below
If you have an issue with a case not being processed properly, or if you're not sure what your best approach to a problem might be - we can help.
Need help to find your way through the insurance process?
Don't worry - it's closer than you think ...
Click here to find out more about Navigators and Counselors
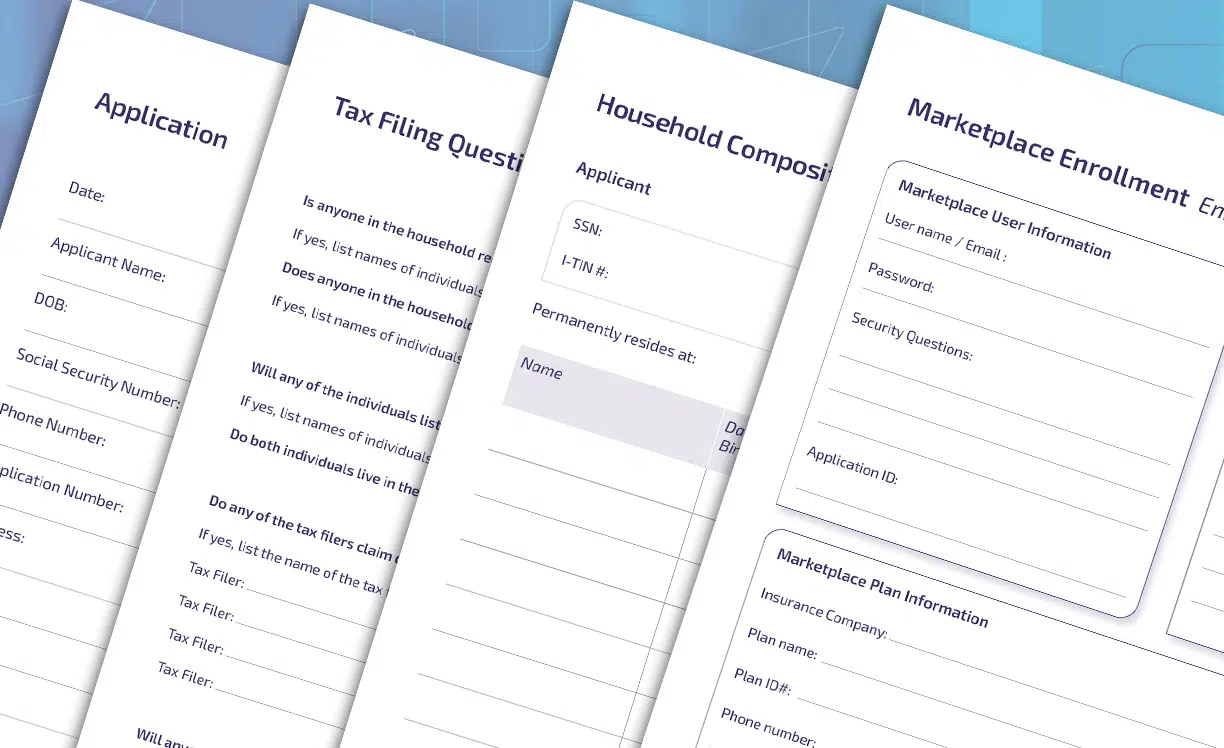
Click here for a set of handy marketplace user forms - application, household compositon, tax questions and more - that you may find useful.
Useful forms to help with Medicaid applications will be added here
- Medicaid phone is 1-800-403—0864
- Medicad Fax 1-888-436-9199
The Health Insurance Marketplace Calculator provides estimates of health insurance premiums and subsidies for people purchasing insurance on their own in health insurance exchanges (or "Marketplaces") created by the Affordable Care Act (ACA). With this calculator, you can enter your income, age, and family size to estimate your eligibility for subsidies and how much you could spend on health insurance.
This interactive tool combines several publicly available data sources to examine how much individuals and families in the United States spend on health each year, both directly and indirectly.

The Plan Year 2026 Assister Certification Training is now available in preparation for Marketplace open enrollment November 1, 2024 - January 15, 2025. Training can be accessed through the CMS Enterprise Portal. The Plan Year 2026 FFM Assister Certification Training Guide provides an overview of how to register as a new assister using the Identity Verification process, or login as a returning assister. Returning assisters should not create another account.
CMS has established Certified Application Counselors (CACs) as a type of assistance personnel trained to provide information to consumers and to help facilitate consumer enrollment in health insurance and insurance affordability programs through the Federally-facilitated Marketplaces (FFMs). In the FFMs, Certified Application Counselor Designated Organizations (CDOs) oversee CACs.
CDOs are a vital component of the assister community.
Click here for more information about the CDO training program

Click here for a selection of short video explainers for some common insurance terms.